loading...
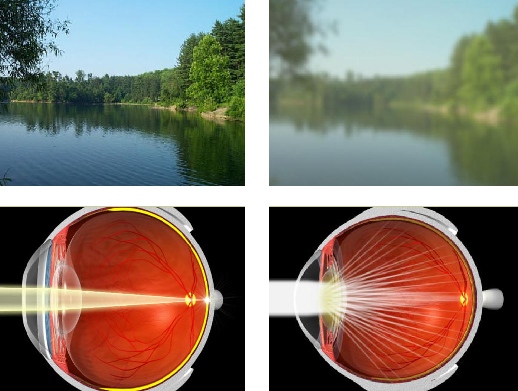
NANDA Definition: Time-limited disruption of sleep (natural, periodic suspension of consciousness) amount and qualitySleep is required to provide energy for physical and mental activities. The sleep-wake cycle is complex, consisting of different stages of consciousness: rapid eye movement (REM) sleep, nonrapid eye movement (NREM) sleep, and wakefulness. As persons age the amount of time spent in REM sleep diminishes. The amount of sleep that individuals require varies with age and personal characteristics. In general the demands for sleep decrease with age. Elderly patients sleep less during the night, but may take more naps during the day to feel rested. Disruption in the individual’s usual diurnal pattern of sleep and wakefulness may be temporary or chronic. Such disruptions may result in both subjective distress and apparent impairment in functional abilities. Sleep patterns can be affected by environment, especially in hospital critical care units. These patients experience sleep disturbance secondary to the noisy, bright environment, and frequent monitoring and treatments. Such sleep disturbance is a significant stressor in the intensive care unit (ICU) and can affect recovery. Other factors that can affect sleep patterns include temporary changes in routines such as in traveling, jet lag, sharing a room with another, use of medications (especially hypnotic and antianxiety drugs), alcohol ingestion, night-shift rotations that change one’s circadian rhythms, acute illness, or emotional problems such as depression or anxiety. This care plan focuses on general disturbances in sleep patterns and does not address organic problems such as narcolepsy or sleep apnea.
Defining Characteristics :
Related Factors :
Expected Outcomes
NOC Outcomes (Nursing Outcomes Classification)
Suggested NOC Labels
NIC Interventions (Nursing Interventions Classification)
Suggested NIC Labels
Ongoing Assessment
Therapeutic Interventions
Education/Continuity of Care
- Verbal complaints of difficulty falling asleep
- Awakening earlier or later than desired
- Interrupted sleep
- Verbal complaints of not feeling rested
- Restlessness
- Irritability
- Dozing
- Yawning
- Altered mental status
- Difficulty in arousal
- Change in activity level
- Altered facial expression (e.g., blank look, fatigued appearance)
Related Factors :
- Pain/discomfort
- Environmental changes
- Anxiety/fear
- Depression
- Medications
- Excessive or inadequate stimulation
- Abnormal physiological status or symptoms (e.g., dyspnea, hypoxia, or neurological dysfunction)
- Normal changes associated with aging
Expected Outcomes
- Patient achieves optimal amounts of sleep as evidenced by rested appearance, verbalization of feeling rested, and improvement in sleep pattern.
NOC Outcomes (Nursing Outcomes Classification)
Suggested NOC Labels
- Anxiety Control
- Sleep
NIC Interventions (Nursing Interventions Classification)
Suggested NIC Labels
- Sleep Enhancement
- Assess past patterns of sleep in normal environment: amount, bedtime rituals, depth, length, positions, aids, and interfering agents. Sleep patterns are unique to each individual.
- Assess patient’s perception of cause of sleep difficulty and possible relief measures to facilitate treatment. For short-term problems, patients may have insight into the etiological factors of the problem (e.g., fear over results of a diagnostic test, concern over a daughter getting divorced, depression over the loss of a loved one). Knowing the specific etiological factor will guide appropriate therapy.
- Document nursing or caregiver observations of sleeping and wakeful behaviors. Record number of sleep hours. Note physical (e.g., noise, pain or discomfort, urinary frequency) and/or psychological (e.g., fear, anxiety) circumstances that interrupt sleep. Often, the patient’s perception of the problem may differ from objective evaluation.
- Identify factors that may facilitate or interfere with normal patterns. Considerable confusion and myths about sleep exist. Knowledge of its role in health/wellness and the wide variation among individuals may allay anxiety, thereby promoting rest and sleep.
- Evaluate timing or effects of medications that can disrupt sleep. In both the hospital and home care settings, patients may be following medication schedules that require awakening in the early morning hours. Attention to changes in the schedule or changes to once-a-day medication may solve the problem.
Therapeutic Interventions
- Instruct patient to follow as consistent a daily schedule for retiring and arising as possible. This promotes regulation of the circadian rhythm, and reduces the energy required for adaptation to changes.
- Instruct to avoid heavy meals, alcohol, caffeine, or smoking before retiring. Though hunger can also keep one awake, gastric digestion and stimulation from caffeine and nicotine can disturb sleep.
- Instruct to avoid large fluid intake before bedtime. This helps patients who otherwise may need to void during the night.
- Increase daytime physical activities as indicated. This reduces stress and promotes sleep.
- Instruct to avoid strenuous activity before bedtime. Overfatigue may cause insomnia.
- Discourage pattern of daytime naps unless deemed necessary to meet sleep requirements or if part of one’s usual pattern. Napping can disrupt normal sleep patterns; however, elderly patients do better with frequent naps during the day to counter their shorter nighttime sleep schedules.
- Suggest use of soporifics such as milk. Milk contains L-tryptophan, which facilitates sleep.
- Recommend an environment conducive to sleep or rest (e.g., quiet, comfortable temperature, ventilation, darkness, closed door). Suggest use of earplugs or eye shades as appropriate.
- Suggest engaging in a relaxing activity before retiring (e.g., warm bath, calm music, reading an enjoyable book, relaxation exercises).
- Explain the need to avoid concentrating on the next day’s activities or on one’s problems at bedtime. Obviously, this will interfere with inducing a restful state. Planning a designated time during the next day to address these concerns may provide permission to "let go" of the worries at bedtime.
- Suggest using hypnotics or sedatives as ordered; evaluate effectiveness. Because of their potential for cumulative effects and generally limited period of benefit, use of hypnotic medications should be thoughtfully considered and avoided if less aggressive means are effective. Different drugs are prescribed depending on whether the patient has trouble falling asleep or staying asleep. Medications that suppress REM sleep should be avoided.
- If unable to fall asleep after about 30 to 45 minutes, suggest getting out of bed and engaging in a relaxing activity. The bed should not be associated with wakefulness.
- For patients who are hospitalized: Provide nursing aids (e.g., back rub, bedtime care, pain relief, comfortable position, relaxation techniques). These aids promote rest.
- Organize nursing care:
- Eliminate nonessential nursing activities.
- Prepare patient for necessary anticipated interruptions/disruptions.
- This promotes minimal interruption in sleep or rest.
- Attempt to allow for sleep cycles of at least 90 minutes. Experimental studies have indicated that 60 to 90 minutes are needed to complete one sleep cycle, and the completion of an entire cycle is necessary to benefit from sleep.
- Move patient to room farther from the nursing station if noise is a contributing factor.
- Post a "Do not disturb" sign on the door.
Education/Continuity of Care
- Teach about possible causes of sleeping difficulties and optimal ways to treat them.
- Instruct on nonpharmacological sleep enhancement techniques.
Nursing Diagnosis for Disturbed Sleep Pattern
Source : http://nursingcareplan.blogspot.com