Diagnosis
Nursing Diagnosis for Impaired Oral Mucous Membrane
NANDA Definition: Disruptions of the lips and soft tissues of the oral cavity Defining Character…
Read moreNursing Diagnosis for Urinary Retention
NANDA Definition: Incomplete emptying of the bladder Defining Characteristics: Measured urina…
Read more5 Nursing Diagnosis for Angina Pectoris
Angina pectoris is a clinical syndrome characterized by episodes or feelings of distress in the ch…
Read more3 Nursing Diagnosis for Pneumonia
Nursing Diagnosis for Pneumonia and Nursing Interventions for Pneumonia 1. Nursing Diagnosis Defi…
Read more4 Nursing Diagnosis for Cholelithiasis
Nanda Nursing Diagnosis for Cholelithiasis 1. Nursing Diagnosis Acute Pain related to: biological …
Read more3 Nursing Diagnosis for Hemophilia
Nursing Diagnosis and Nursing Interventions for Hemophilia 1. Nursing Diagnosis: Ineffective Tissue…
Read moreNursing Diagnosis for Self Care Deficit
Nursing Diagnosis: Self-Care Deficit Bathing/Hygiene; Dressing/Grooming; Feeding; Toileting NANDA D…
Read more10 Nursing Diagnosis for Chronic Obstructive Pulmonary Disease (COPD)
10 List of Nanda Nursing Diagnosis for COPD 1. Ineffective airway clearance related to: bro…
Read moreSearch This Blog
Popular Posts
5 Nursing Diagnosis for Gastritis
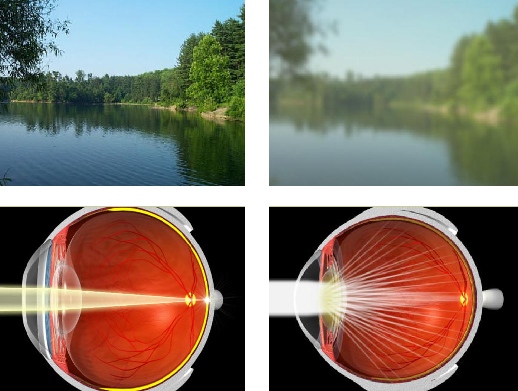
4 Nursing Diagnosis for Cataracts

